Bench to Bedside? Breastfeeding Best Practices Embrace Social Science
Emerging empirical research from chemistry, microbiology, animal science, nutrition, pediatrics, and evolutionary anthropology are accelerating our understanding of the magic of milk. Translating the findings about milk, however, for the end-user (babies) and end-producers (moms), requires shining a light on emerging social science and public health research tackling breastfeeding initiation and support. Moreover, understanding the context and experiences of mothers of different races highlights the persistence of health care deficits that perpetuate breastfeeding disparities.
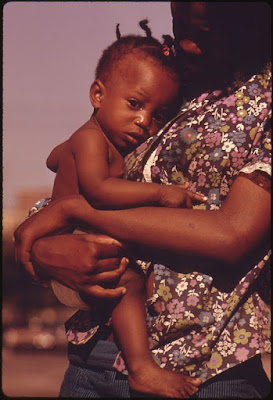
John H. White, National Archives
Demographics & Epidemiology
In 2014, Dr. Lind and colleagues evaluated the maternity and perinatal practices at 2,227 hospitals and birth centers in the United States in conjunction with the racial demographics of the area served by these health care facilities (1). Combining data from the CDC’s 2011 Maternity Practices in Infant Nutrition and Care survey with census data on racial demographics in the same zip code as the health facilities, the authors discovered failures of health care delivery in communities with higher proportions of Black residents.
Early initiation of breastfeeding within the first hour of an uncomplicated vaginal birth, rooming-in, and post-discharge patient support were all less likely to be standard practice in zip codes in which Black residents were >12.2% of the population. Facilities serving these communities were also less likely to limit the use of breastfeeding supplements. These are four of the ten important steps toward optimal support for breastfeeding and mother and infant bonding. Together these practices underlie the Baby-Friendly Hospital Initiative and have been demonstrated to improve breastfeeding initiation and success, including among Black women (2).
More recent research by Dr. McKinney and colleagues investigated differences among white, Hispanic, and Black mothers in breastfeeding initiation and duration (3). Using a large sample (N=1636) of mothers from the Community and Child Health Network, a multi-community project of the National Institutes of Health, McKinney replicated previously-demonstrated patterns of disparity between white and Black mothers, 78% vs. 61% initiation respectively. Hispanic mothers had the highest initiation with more than 90% initiating breastfeeding. The disparity between white and Black mothers was explained by poverty, college education, and marital status as white mothers were wealthier, more likely to be college-educated, and more likely to have a spouse. Although Hispanic and Black mothers had similar socioeconomic and demographic backgrounds, the higher initiation among Hispanic women reflected a family history of breastfeeding (3).
Tamara Adams
For the mothers who initiated breastfeeding, however, these socioeconomic and demographic factors, however, could not alone explain differences in breastfeeding duration among these groups (3). Hispanic mothers breastfed 10 and 17 weeks (English-speaking and Spanish-speaking, respectively) while white mothers breastfed on average 16.5 weeks and Black mothers breastfed only 6.4 weeks. The introduction of formula-feeding during the hospital stay was a significant predictor for the disparity between white and Black mothers in breastfeeding duration.
The authors concluded that “if only hospital formula introduction were eliminated, the black/white gap in breastfeeding duration could be reduced by ∼1.8 weeks, 20% of the overall difference.”
Taking a Closer Look
The above quantitative analyses are importantly complimented by qualitative, ethnographic approaches to understanding the socio-cultural context of infant-feeding decisions. In August, Dr. Ifeyinwa Asiodu and colleagues published the results from a “critical ethnographic” approach to infant-feeding among first-time African American mothers (4). Critical ethnography moves beyond earlier forms of cultural description, to specifically capture the complex factors and their intersections that contribute to observed societal disparities. This research method provided rich detail that informs “culturally inclusive messaging” in public health and clinical practice.
Over the course of many interviews, mothers and members of their support networks described the factors related to breastfeeding initiation and success. Consistent with the quantitative work of McKinney et al. (3), Asiodu and colleagues found that a family history of breastfeeding among African-American women was rare, but if present improved breastfeeding initiation. Moreover a mother’s broader social networks, and the support or lack of support therein, could improve or reduce breastfeeding practices. Motherhood as a critical aspect of self-identity was also a motivating factor in breastfeeding and infant nurturing. Lastly, access to community public health programs that provided support, information, and facilitated new mothers connecting with other new mothers also contributed importantly to breastfeeding practices and attitudes (4).
mizchartreuse
Understanding the importance and cultural context of female social networks for shaping breastfeeding practices contributes to adopting best practices in the clinical setting, namely implementing peer-mentor programs. Dr. Paula Meier and colleagues at the Rush University Medical Center (RUMC) in Chicago have established the Rush Mothers’ Milk Club in the NICU that provides a roadmap for building partnerships among many stakeholders to promote breastfeeding (5). From the clinical staff, to the families and patients, to the broader community members in the neighborhood surrounding the RUMC, the core principle of the program is “sharing the science of human milk and lactation with NICU families so that the families could serve as active participants in their infants’ feeding decisions and management plans” (5).
Within a year of launching this program, breastfeeding initiation rates for mothers with babies in the NICU went from 17% to 95% as mothers decided to breastfeed after hearing about “milk as medicine for their baby” (5). The mothers most likely to change their infant-feeding decision from formula-feeding to breast milk-feeding were low-income, African American mothers who had particularly vulnerable small, pre-term infants and who had few, if any, breastfeeding models within their existing social support networks (5).
Informal mother-to-mother peer-counseling was an emergent dynamic during weekly Rush Mother’s Milk Club meetings, and inspired a peer-mentoring network. Breastfeeding peer counselors, who had themselves had a baby in the NICU, became valuable role models and sources of information for mothers whose existing social support network had little information about breastfeeding—especially small, premature infants, particularly for African American mothers (5).
Moving Forward
These studies at the social science/life science/clinical practice interface reveal key gaps, but also provide solutions for addressing persistent health care disparities. Life scientists are prioritizing understanding how early life organization can exert life-long consequences (6, 7), a field known as the Developmental Origins of Health and Disease (7). At the same time, researchers in the social sciences are investigating how babies born in nearby zip codes can have 20-30 year differences in their life expectancy because of deficits in the quality of care and disparities of life experiences (8). Due to inadequate breastfeeding support and therefore breastfeeding initiation and success, more Black mothers and babies are likely to accrue compounding health effects throughout the lifetime and across generations (8).
Indeed, epidemiological models published in Fall 2016 by Dr. Melissa Bartick, Dr. Alison Steube and colleagues reveal that the racial breastfeeding gap is associated with poorer health for non-Hispanic Blacks than non-Hispanic whites (9). Non-Hispanic blacks experienced over 3x greater incidence of necrotizing enterocolitis (NEC) and over 2x higher infant mortality attributable to reduced breastfeeding rates (9). Earaches and other gastrointestinal disorders were also more common as a result of breastfeeding disparities for non-Hispanic Blacks than non-Hispanic whites (9). These higher incidences of illness were associated with greater medical costs, but likely also contribute to missed work and lost income, worsening the impacts of breastfeeding disparities (9).
As evidenced by the articles cited here, the development and adoption of emergent and evidence-based approaches, tools, and interventions within health delivery settings require more frequent collaboration among life and social scientists. In other words, social science is a key component to the translation of bench science to patient care.
Citations
1. Lind, Jennifer N., Cria G. Perrine, Ruowei Li, Kelley S. Scanlon, and Laurence M. Grummer-Strawn. "Racial disparities in access to maternity care practices that support breastfeeding—United States, 2011." MMWR Morb Mortal Wkly Rep 63, no. 33 (2014): 725-728.
2. Philipp, Barbara L., Anne Merewood, Lisa W. Miller, Neetu Chawla, Melissa M. Murphy-Smith, Jenifer S. Gomes, Sabrina Cimo, and John T. Cook. "Baby-friendly hospital initiative improves breastfeeding initiation rates in a US hospital setting." Pediatrics 108, no. 3 (2001): 677-681.
3. McKinney, Chelsea O., Jennifer Hahn-Holbrook, P. Lindsay Chase-Lansdale, Sharon L. Ramey, Julie Krohn, Maxine Reed-Vance, Tonse NK Raju, and Madeleine U. Shalowitz. "Racial and ethnic differences in breastfeeding." Pediatrics 138, no. 2 (2016): e20152388.
4. Asiodu, Ifeyinwa V., Catherine M. Waters, Dawn E. Dailey, and Audrey Lyndon. "Infant Feeding Decision-Making and the Influences of Social Support Persons Among First-Time African American Mothers." Maternal and Child Health Journal (2016): 1-10.
5. Meier, Paula P., Janet L. Engstrom, and Beverly Rossman. "Breastfeeding peer counselors as direct lactation care providers in the neonatal intensive care unit." Journal of Human Lactation (2013): 0890334413482184.
6. Thayer, Z. M., & Kuzawa, C. W. (2014). Early origins of health disparities: Material deprivation predicts maternal evening cortisol in pregnancy and offspring cortisol reactivity in the first few weeks of life. American Journal of Human Biology, 26(6), 723-730.
7. Rubin, Lewis P. "Maternal and pediatric health and disease: integrating biopsychosocial models and epigenetics." Pediatric research (2015).
8. Graham, Garth N. "Why Your ZIP Code Matters More Than Your Genetic Code: Promoting Healthy Outcomes from Mother to Child." Breastfeeding Medicine 11, no. 8 (2016): 396-397.
9. Bartick, Melissa C., Briana J. Jegier, Brittany D. Green, Eleanor Bimla Schwarz, Arnold G. Reinhold, and Alison M. Stuebe. "Disparities in Breastfeeding: Impact on Maternal and Child Health Outcomes and Costs." The Journal of Pediatrics (2016).
Note: Terms for race designations, such as “Black” and “African-American,” came directly from the articles cited. These terms were capitalized in accordance with recommendations from Halley, J., Eshleman, A., & Vijaya, R. M. (2011). Seeing white: An introduction to white privilege and race. Rowman & Littlefield Publishers.
An earlier version of this essay appeared in SPLASH! Milk Science Update








Comments
Post a Comment